When you’re taking anticoagulants, it’s amazing how quickly you pick up medical jargon, especially if it’s related to your own condition,
But as these acronyms cover all conditions related to coagulation there will probably be some you don’t know.
Take our quiz and see if your score out of ten makes you
Coagulation Conqueror (Score 7+),
Coagulation Competent (Score 4-6) or
Coagulation Crisis (Score 3 or less)
An easy one to start with; Deep Vein Thrombosis is a bread-and-butter condition for this site!
These clots form in veins deep inside the leg. The veins involved cannot be seen.
DVTs most commonly form in the leg veins but can occur in other parts of the body such as the arms or intestines.
Your doctor may suspect that you have a deep vein thrombosis if you have some of the following symptoms.
- Pain – this can be anywhere in the leg but is commonly felt in the calf.
- Swelling – often most obvious around the ankle, but can involve the whole leg.
- Redness – a slight dusky discolouration of the leg is common.
- Warmth – the leg feels warm to touch.
These are the most common symptoms of a deep vein thrombosis but they are not all present in all cases.
electro-cardiogram. (In America it’s called an EKG, I’m not sure why as I think they write ‘cardio’ rather than ‘kardio’ for things associated with the heart). This is a tracing of the electrical activity of the heart.
There are 3 main links between ECG and blood clots.
An ECG can show if there’s a disorder of heart rhythm, as with the ECG shown which is of AF, atrial fibrillation, the commonest reason for being on warfarin. If you have AF, there’s the potential for a clot to form in the atria of the heart then break away to lodge in the brain and cause a stroke.
An ECG can also show if there is damage to the heart muscle as occurs after a heart attack when a blood clot forms in one of the vessels of the heart, blocking the blood supply to the muscle.
Very occasionally pulmonary embolism shows up as a specific pattern on an ECG.
The commonest reason for replacing the mitral valve of the heart is because it leaks. If the replacement valve is a mechanical one, you need to take an anticoagulant long-term to prevent clots. This is because the foreign material in the valve is in contact with your blood. This stimulates the clotting process and can lead to a blood clot forming on the valve. This can be very dangerous and lead to a stroke.
Warfarin is the only suitable anticoagulant to take after heart valve surgery, the newer anticoagulants are not as safe for this condition.
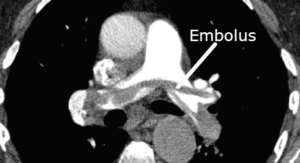
CTPA stands for Computerised tomographic Pulmonary angiogram. This test looks for pulmonary embolism.
A pulmonary embolus (PE) occurs when part of a blood clot somewhere else in the body breaks off and travels to the lungs. The embolus could come from a deep vein thrombosis in the leg or the pelvis. The floating piece of clot blocks the blood supply to the lungs. A small pulmonary embolus may not cause any symptoms, but a large one can cause breathing difficulties, fainting spells and can even be fatal.
This is the most common heart-valve procedure and is usually because the aortic valve has become narrowed and prevented normal blood flow. As with mitral valve replacement, if the replacement valve is a mechanical one, you need to take an anticoagulant long-term to prevent clots. Warfarin is the only suitable anticoagulant to take after heart valve surgery, the newer anticoagulants are not as safe for this condition.
Community pharmacy Anticoagulation Management Service. A tricky one if you live outside NZ!
In NZ, 6,000 people use this service to manage their warfarin through 150 pharmacies.
- When their INR test is due, they go to their local pharmacy instead of the laboratory for the blood test, which uses a finger-prick sample.
- The test results are available immediately, and the pharmacist can tell them straight away the correct dose of warfarin to take. A small calendar is printed off for them to take away showing them what dose of warfarin to take each day.
- The GP is informed immediately of the INR result, and is able to make any changes to the recommended dose, if needed. The GP still has the overall responsibility for peoples’ care.
Providing the INR Online software to the CPAMS service is how this site is funded.
New Oral Anticoagulants or Novel Oral anticoagulants. There has been a lot of discussion about what these drugs should be called as they are no longer “New”. Obviously there are many old things that are still called new, for example New Zealand and New York, but the present view is we should call these new drugs DOACs, which stands for Direct Oral antcoagulants. The direct refers to how they work as direct inhibitors of specific clotting factors. The DOACs available are dabigatran (Pradaxa), rivaroxaban (Xarelto), apixaban (Eliquis) and edoxaban (Savaysa).
The traditional anticoagulants are warfarin pills and heparin (clexane) injections
When I teach medical students about the INR I give them a few options for what INR stands for including
I‘m Not Really sure
I Never Read that chapter
Irrationally Named Ratio
but INR actually stands for the International Normalised Ratio. This is a ratio of how long blood takes to clot from somebody taking warfarin compared to somebody not taking warfarin. For example if your blood takes 20 secs to clot and somebody not on warfarin takes 10 secs the INR is 2.0. The international normalised part is a correction for the reagents used to do the test in the lab, so if you got an INR test in New Zealand the results should be the same in the USA even though different labs use different reagents.
Another of the core diagnoses covered by this site; atrial fibrillation. This is the commonest reason for being on anticoagulants.
Atrial fibrillation is an abnormal rhythm of the heart. It can be an intermittent (paroxysmal) or chronic condition.
In atrial fibrillation the upper chambers of the heart (or atria) do not work correctly because of abnormal electrical activity. Blood is not forcefully moved out of these chambers and becomes ‘static’, which allows blood clots to form and can put patients at risk of stroke.
Atrial fibrillation often occurs in people who have underlying heart disease. Almost any heart disease can increase the risk of this abnormal rhythm, but the most common causes are:
- Hypertensive heart disease due to chronic high blood pressure.
- A heart attack (myocardial infarction, or MI)
- Heart failure
[collapse]



Leave a Reply