Deep vein thrombosis
 The diagnosis of a DVT in pregnancy is made using similar methods to those used in women who are not pregnant, but the d-dimer test is not so reliable. The d-dimer measures the breakdown products of blood clot. It is used to exclude a blood clot so people with a low level have a low risk of a blood clot. However the baseline level of the d-dimer in the blood goes up during pregnancy making it a less useful test. Therefore any woman with a suspected DVT in pregnancy should have an ultrasound scan. A positive scan confirms the diagnosis. If the scan is negative and your doctor is still suspicious that you may have a clot, you should have a repeat ultrasound a few days later.
The diagnosis of a DVT in pregnancy is made using similar methods to those used in women who are not pregnant, but the d-dimer test is not so reliable. The d-dimer measures the breakdown products of blood clot. It is used to exclude a blood clot so people with a low level have a low risk of a blood clot. However the baseline level of the d-dimer in the blood goes up during pregnancy making it a less useful test. Therefore any woman with a suspected DVT in pregnancy should have an ultrasound scan. A positive scan confirms the diagnosis. If the scan is negative and your doctor is still suspicious that you may have a clot, you should have a repeat ultrasound a few days later.
A clot in the pelvis is not always detected with ultrasound and magnetic resonance venography may be necessary to confirm a clot.
Pulmonary embolus
The main concern about diagnosing a pulmonary embolus in pregnancy is the risk to the baby and you from the radiation used in the investigations. All women with a suspected PE should have a chest X-Ray, this only 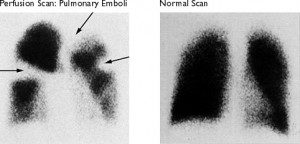 exposes the baby to a very small dose of radiation and is generally regarded as safe. The X-Ray can help your doctor decide which test to do next. If you have symptoms of a DVT as well as PE you should have an ultrasound of your legs first. If this confirms a blood clot you do not need any more investigations and should be treated for the clot. If the ultrasound is negative or you do not have any leg symptoms you will need either a CT Pulmonary angiogram or a Ventilation/Perfusion scan (V/Q scan).
exposes the baby to a very small dose of radiation and is generally regarded as safe. The X-Ray can help your doctor decide which test to do next. If you have symptoms of a DVT as well as PE you should have an ultrasound of your legs first. If this confirms a blood clot you do not need any more investigations and should be treated for the clot. If the ultrasound is negative or you do not have any leg symptoms you will need either a CT Pulmonary angiogram or a Ventilation/Perfusion scan (V/Q scan).
CTPA or Ventilation perfusion scan?
 Both of these scans expose the baby to a low level of radiation. There is a lot of debate about which has the lowest exposure but the Royal College of Obstetricians and Gynaecologists guidelines quote an exposure of 0.1mGy for a CTPA and 0.5mGy for a V/Q scan. There is no immediate risk to the baby but some studies suggest that radiation in utero can increase the risk of cancer in childhood. Again this is a very low risk; about 1 in 17,000 per mGy of exposure. Many doctors believe that the CTPA is more useful as it will often show up other problems, for example if you have chest pain the doctor may suspect a PE but the scan might pick up pneumonia.
Both of these scans expose the baby to a low level of radiation. There is a lot of debate about which has the lowest exposure but the Royal College of Obstetricians and Gynaecologists guidelines quote an exposure of 0.1mGy for a CTPA and 0.5mGy for a V/Q scan. There is no immediate risk to the baby but some studies suggest that radiation in utero can increase the risk of cancer in childhood. Again this is a very low risk; about 1 in 17,000 per mGy of exposure. Many doctors believe that the CTPA is more useful as it will often show up other problems, for example if you have chest pain the doctor may suspect a PE but the scan might pick up pneumonia.
Breast cancer risk
The down side to the CTPA is the high radiation exposure to the pregnant breast tissue, the exposure is about 20 times higher than with a V/Q scan and is up to 20mGy. Breast tissue is particularly sensitive to radiation in pregnancy and the risk is highest for younger women. For a 25-year-old whose background risk of developing breast cancer in the following 10 years is 0.1%, the extra risk from 10mGy of radiation increases the risk by 13.6% of 0.1%, which is 0.0136% extra. This remains a low risk but it is prudent to consider a V/Q scan if you are young especially if you have a family history of breast cancer.

Valuable blog article, it was quite interesting nice work. I want to thank you for this informative read, I really appreciate sharing your post. This is my great pleasure to visit your website and to enjoy your excellent post here.