In this Medical Monday series, we’re talking about how your doctor reaches a diagnosis of common conditions associated with coagulation. It may help if you first read the introduction and the topic of pulmonary embolism, before reading about today’s topic of pulmonary hypertension. Altogether we’re covering
- Introduction
- DVT, Deep Vein Thrombosis
- Post-thrombotic syndrome
- PE, Pulmonary Embolism
- Pulmonary hypertension
- AF, Atrial Fibrillation
- Heart Valve conditions – aortic and mitral
- Thrombophilia
- Stroke
Introduction
Pulmonary hypertension is a type of high blood pressure in the blood vessels in the lungs. There are many causes of pulmonary hypertension including lung disease and blood vessel problems, but in a large number of people the cause remains unknown. One type of pulmonary hypertension that is relevant to people who have had pulmonary emboli, is a condition called chronic thromboembolic pulmonary hypetension (CETPH or WHO Group IV pulmonary hypertension) which is due to repeated pulmonary emboli blocking the arteries in the lung. This means your heart has more work to do to push blood through the lungs. The right side of the heart can compensate for a while but eventually starts to fail.
Your story
 Pulmonary hypertension can come on slowly often over many years. The symptoms are increasing breathlessness, first with exercise but later you can become breathless at rest. It also leads to fatigue and occasional dizzy spells. If the heart is under strain your pulse rate can increase and your ankles swell. Late in the disease it is harder to fully oxygenate your blood and your lips can go slightly blue. There are some people who have repeated pulmonary emboli and don’t realise they have had them. It is a very serious condition that unfortunately affects young people. The type of pulmonary hypertension related to blood clots can improve with treatment so it is important that it is diagnosed early.
Pulmonary hypertension can come on slowly often over many years. The symptoms are increasing breathlessness, first with exercise but later you can become breathless at rest. It also leads to fatigue and occasional dizzy spells. If the heart is under strain your pulse rate can increase and your ankles swell. Late in the disease it is harder to fully oxygenate your blood and your lips can go slightly blue. There are some people who have repeated pulmonary emboli and don’t realise they have had them. It is a very serious condition that unfortunately affects young people. The type of pulmonary hypertension related to blood clots can improve with treatment so it is important that it is diagnosed early.
Questions your doctor may ask
Pulmonary hypertension can be very difficult to pick up. Your doctor will be particularly interested in the progression of your symptoms; breathing gets gradually worse and the fatigue becomes more obvious. You may also be asked about a history of blood clots or a family history of pulmonary hypertension. You doctor will also want to know about your medication, especially any recreational drugs; amphetamines and cocaine have been linked to this condition. It is also worse if you have sleep apnoea or if you are a smoker.
What your doctor may find
 Your doctor may not find any abnormality until the condition is quite advanced and even then the findings are not specific for the condition. You may have an increased heart rate and slight ankle swelling. When doctors listen to your heart, they may find some specific signs such as a loud second heart sound and a murmur from a leaking pulmonary valve, but these are very hard to pick up. Your doctor may also look at your neck to see if the central venous pressure is raised, this is called the jugular venous pressure or JVP. It will be high in pulmonary hypertension.
Your doctor may not find any abnormality until the condition is quite advanced and even then the findings are not specific for the condition. You may have an increased heart rate and slight ankle swelling. When doctors listen to your heart, they may find some specific signs such as a loud second heart sound and a murmur from a leaking pulmonary valve, but these are very hard to pick up. Your doctor may also look at your neck to see if the central venous pressure is raised, this is called the jugular venous pressure or JVP. It will be high in pulmonary hypertension.
Tests you may have
 Your doctor will do a chest X-ray, an ECG and some blood tests. The X-ray is to see if there is any underlying lung problem and it might show an enlarged right side of the heart, the ECG may also show some enlargement of the right sided heart chambers. The blood tests are to exclude autoimmune diseases and infections like HIV.
Your doctor will do a chest X-ray, an ECG and some blood tests. The X-ray is to see if there is any underlying lung problem and it might show an enlarged right side of the heart, the ECG may also show some enlargement of the right sided heart chambers. The blood tests are to exclude autoimmune diseases and infections like HIV.
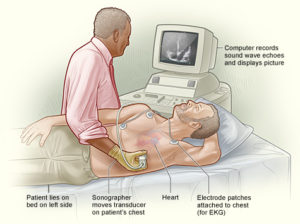
The most important test is an echo cardiogram. This is like an ultrasound scan of your heart and shows the size of the chambers and can be used to measure the pressures in the heart. If this is abnormal you may be asked to have more detailed tests of lung function and oxygen consumption. You may also need a CT or MRI scan of your lungs. One simple test that is used to monitor progress of the disease is the “six minute walk” test, basically this is the distance you can walk in 6 minutes.
What else it could be
- Fatigue is a very common symptom and there are many causes including side-effects of many medications.
- The increased heart rate and ankle swelling are symptoms of a variety of heart conditions and breathlessness is also non-specific.
Don’t panic!
Many people feel tired after a pulmonary embolus, this does not mean you are developing pulmonary hypertension. But if you have had more than one blood clot and you no longer take an anticoagulant it is important to be aware of this condition.
Warfarin is one of the treatments for this condition and does improve the outcome if it is due to blood clots.

Leave a Reply